Non-enzymatic Ex-vitro Antioxidant, Biosafety, Analgesic and Anti-inflammatory Evaluation of Aqueous Polyherbal (ELNA) Extract in Mice.
Main Article Content
Abstract
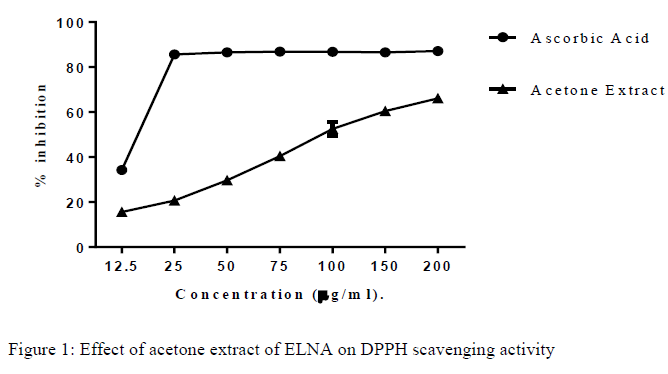
The polyherbal formulation known as ELNA consists of Moringa oleifera, Crateva religiosa and Curcuma longa. It ethnomedicinal properties include; analgesic, inflammation, cardiac diseases, bacterial infection and immune suppressed diseases. The aim of this study was to evaluate the ex-vitro non-enzymatic anti-oxidant, biosafety, analgesic and anti-inflammatory effect of aqueous ELNA polyherbal extract. Ex-vitro anti-oxidant study was investigated in ELNA extract using standard radical scavenging protocol. Biosafety effect of ELNA extract was understudied with the aid of Locke method. Acetic acid-induced peripheral pain, hot plate-induced central pain and egg albumin-induced inflammatory models were investigated. Results from this study exhibited the scavenging effect of ELNA extract against 1, 1-diphenyl-2-picryhydroxyl with significant increase in concentration dependent manner. Acute toxicity study of the aqueous extract of ELNA elicited less or no toxic effect, with no mortality and side effect above LD50>5000 mg/kg body weight. Aqueous ELNA extract displayed no damaging effect of the sub-chronic toxicity study administered for 28 days, exhibited no significant difference (p= 0.05) in the organ and body weight. No significant different in the haematological parameters excluding 400 mg/kg with slight significant (p<0.05) increase in platelet count. Graded doses of the extract at 400, 800 and 1200 mg/kg body weight exhibited significant (p<0.05) reduction in central and peripheral pain. Significant reduction in paw edema volume. Specifically at higher doses, the extract showed an effective activities against the selected study. In conclusion, this study validated the ethnomedicianl evidence of ELNA aqueous extract of the formulation.
Article Details
References
Barnes, J., Anderson, L. A., Phillipson, J. D. Herbal Medicine. 3rd Edition, Pharmaceutical Press, London. 2007, pp. 1-23.
WHO. WHO Monographs on Selected Medicinal Plants, World Health Organization, Geneva. 2002a, 2.
Chandraprakash, D., Swarnali, D. Anti-diabetic herbal drugs and polyherbal formulation used for diabetes: A review. Journal of Phytopharmacology. 2013, 2(3): 44-51. DOI: https://doi.org/10.31254/phyto.2013.21308
Gomase, P., Shire, S. P., Nazim, S., Choudhari, A. B. Development and evaluation of polyherbal formulation for anti-inflammatory activity. Journal of Natural Product and Plant Resource. 2011, 1: 85-90.
Sies, H. Oxidative stress: Oxidant and anti-oxidant. Experimental Physiology. 1997, 82(2): 291–295. DOI: https://doi.org/10.1113/expphysiol.1997.sp004024
Cadenas, E. Basic mechanisms of antioxidant activity. Biofactors. 1997, 6: 391–397. DOI: https://doi.org/10.1002/biof.5520060404
Oyewole, I. O., Magaji, Z. J., Awoyinka, O. A. Biochemical and toxicological studies of aqueous extract of Tithonia diversifolia leaves in Wister albino rats. Journal of Medicinal Plants Research. 2007, 1: 30-33.
O’Hara, M. A., Kiefer, D., Farrell, K., Kemper, K. A review of 12 commonly used medicinal herbs. Archive of Family Medicine. 1998, 7: 523-536. DOI: https://doi.org/10.1001/archfami.7.6.523
Hayes, A. W. Histologic changes in the respiratory tract induced by inhalation of xenobiotics: Physiologic adaptation or toxicity? Toxicology and Applied Pharmacology. 1989, 101: 521–542. DOI: https://doi.org/10.1016/0041-008X(89)90200-7
Rang, H. P. Dale, M. M. Harmful effects of Drugs In: Rang H. P and Dale, M.M. (Eds.) Rang and Dales Pharmacology 6th edition Churchill Livingstone USA. 2007, pp. 752 – 764. DOI: https://doi.org/10.1016/B978-0-443-06911-6.50058-X
Giordano, J. The neurobiology of nociceptive and antinociceptive systems. Pain Physician. 2005, 8: 277-290. DOI: https://doi.org/10.36076/ppj.2005/8/277
Spanswick, C. C., Main, C. J. Pain Management: An interdisciplinary approach. Edinburgh: Churchill Livingstone. 2000, 93p.
Urch, C. E., Suzuki, R. Pathophysiology of Somatic, Visceral and Neuropathic Cancer Pain. In: Sykes, N., Bennett, M. I., Yuan, C. S. Clinical pain management: Cancer pain. 2nd Ed. London: Hodder Arnold. 2009, pp. 3-14. DOI: https://doi.org/10.1201/b13440-1
Stein, C. The control of Pain in Peripheral Tissues by Opioids. Journal of Medicine. 1995, 332: 1685-1690. DOI: https://doi.org/10.1056/NEJM199506223322506
Vranken, J. H. Mechanism and treatment of neuropathic pain. Central Nervous System Agents in Medicinal Chemistry. 2009, 9(1): 73-77. DOI: https://doi.org/10.2174/187152409787601932
Cotran, K. C. Robbins Pathologic Basis of Disease. Philadelphia: W.B. Saunders Company. 1998, pp. 152-170.
Lorke, D. A new approach to practical acute toxicity testing. Archives of Toxicology 1983, 54: 275-287. DOI: https://doi.org/10.1007/BF01234480
Nakamura, H., Shimoda, A, Ishii, K., Kadokawa, T. Central and peripheral analgesic action of non-acidic non-steroidal anti-inflammatory drugs in mice and rats. Archives of International Pharmacodynamics. 1986, 282: 16–25.
Eddy, N. B., Touchberry, C. F., Lieberman, I. E. Synthetic analgesics, a methadone isomers and derivatives. Journal of Pharmacology and Experimental Therapeutics. 1950, 98: 121-137.
Winter, E. R., Risley, E. A., Nuss, G. V. Anti-inflammatory and anti-pyretic activities of indomethacin. Journal of pharmacology. 1963, 141: 369-376.
Akah, P. Nwabie, A. I. Evaluation of Nigerian traditional medicines: Plants used for rheumatic disorder. Journal of Ethnopharmacology. 1994, 42: 179-182. DOI: https://doi.org/10.1016/0378-8741(94)90083-3
Iwu, M. M. Handbook of African Medicinal Plants. CRC Press, London. 1993, pp. 183-184.
Siddhuraju, P., Becker, K. Antioxidant properties of various solvent extracts of total phenolic constituents from three different agroclimatic origins of drumstick tree (Moringa oleifera Lam.) leaves. Journal of Agricultural and Food Chemistry 2003, 51: 2144-2155. DOI: https://doi.org/10.1021/jf020444+
Singh, B. N., Singh, B. R., Singh, R. L., Prakash, D., Dhakarey, R., Upadhyay, G., Singh, H. B. Oxidative DNA damage protective activity, antioxidant and anti-quorum sensing potentials of Moringa oleifera. Food Chemistry and Toxicology 2009, 47: 1109-1116. DOI: https://doi.org/10.1016/j.fct.2009.01.034
Vaghasiya, Y. K., Shukla, V. J., Chanda, S. V. Acute oral toxicity study of Pluchea argutaboiss extract in mice. Journal of Pharmacology and Toxicology. 2011, 6: 113-123. DOI: https://doi.org/10.3923/jpt.2011.113.123
Ukwuani, A. N., Abubakar, M. G., Hassan, S. W., Agaie, B. M. Toxicological studies of hydromethanolic leaves extract of Grewi acrenata. International Journal of Pharmaceutical Science and Drug Research. 2012, 4: 245–249.
Adamu, A., Abdurrrahman, E. M., Ibrahim, H., Abubakar, M. S., Magaji, M. G., Yaro, A. H. Effect of Aqueous methanolic stem of bark extract of Maerua angolensison acute and sub-acute inflammations. Nigerian Journal of Pharmaceutical Sciences. 2007, 6(2): 1-6.
Chainani-Wu, N. Safety and anti-inflammatory activity of curcumin: a component of tumeric (Curcuma longa). Journal of Alternative and Complementary Medicine. 2003, 9(1): 161–168. DOI: https://doi.org/10.1089/107555303321223035
Tripathy, S. A., Ashaa, M. D. Pradhanaacute and chronic anti-inflammatory evaluation of crateva religiosa in rats. International Journal of Pharmacy and Technology. 2010, 2(4): 1270-1279.
Awodele, O., Oreagba, I. A., Odoma, S., da Silva, J. A., Osunkalu, V. O. Toxicological evaluation of the aqueous leaf extract of Moringa oleifera Lam. (Moringaceae). Journal of Ethnopharmacology. 2012, 139(2): 330-336. DOI: https://doi.org/10.1016/j.jep.2011.10.008
Sireeratawong, S., Urarat, N., Supaporn, V., Natthakarn, C., Supachai, S., Pennapa, S., Pornthip, T., Parunkul, C., Kanjana, J. Acute and subchronic toxicity study of tud-rak-ka-sai-puu recipe in rats. African Journal of Traditional, Complementary and Alternative Medicine 2013, 10(1):142-148. DOI: https://doi.org/10.4314/ajtcam.v10i1.19
Gene, R. M., Segura, L., Adzet, T., Marin, E., Iglesias, J. Heterotheca inuloides: Anti-inflammatory and analgesic effects. Journal of Ethnopharmacology. 1998, 60: 157-162. DOI: https://doi.org/10.1016/S0378-8741(97)00155-4
Tanko, Y., Magaji, G., Yerima, M., Magaji, A., Mohammed, A. Antinociceptive and anti-inflammatory activities of aqueous leaves extract of Ocimum gratissimum (Labiatea) in rodents. African Journal of Traditional, Complementary and Alternative Medicines. 2008, 5(2): 141-146. DOI: https://doi.org/10.4314/ajtcam.v5i2.31265
Santosh, S., Sohan, S., Anupana, S., Devanand, S., Manohar, J.P. Anti-inflammatory activity of an isolated flavonoid fraction from Celosia argentea Linn. Journal of Medicinal Plants Research. 2008, 2(3): 52-54.
Zakaria, Z., Sulaiman, M., Gopalan, H., Ghani, Z., Raden-Mohd, R., Jais, M., Abdullah, F. Anti-nociceptive and anti-inflammatory properties of Corchorus capsularis leaves chloroform extract in experimental animals models. Journal of the Pharmaceutical Society of Japan 2007, 127: 359-365. DOI: https://doi.org/10.1248/yakushi.127.359
Ferdous, M., Rouf, R., Shilpi, J., Uddin, S. Antinociceptive activity of aqueous extract of Ficus racemosa linn. Oriental Pharmacy and Experimental Medicine. 2008, 8: 93-96. DOI: https://doi.org/10.3742/OPEM.2008.8.1.093
Kumar, Y., Vanitha, K., Prakash, K., Swetha, M. A new facile and sensitive method for the estimation of tapentadol. International Journal of Pharmaceutical Sciences and Drug Research. 2014, 6(1): 82-84.
Akindele, A. J, Adeyemi, O. O. Anti-inflammatory activity of the aqueous leaf extract of Byrsocarpus coccineus. Fitoterapia. 2007, 78: 25-28. DOI: https://doi.org/10.1016/j.fitote.2006.09.002
Wannang, N. N., Anuka, J. A., Kwanashie, H. O., Auta, A. Analgesic and anti-inflammatory activity of the aqueous leaf extract of Solanum nigrum Linn (Solanaceae) in Rat. Nigerian Journal of Pharmaceutical Research. 2006, 5: 9-13. DOI: https://doi.org/10.4314/njpr.v5i1.53546